Brachial
Plexus Injuries
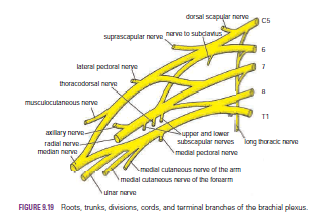
The roots, trunks, and divisions of the brachial plexus
reside in the lower part of the posterior triangle of the neck, whereas the cords
and most of the branches of the plexus lie in the axilla.
Complete lesions involving all the roots of the plexus are
rare.
Incomplete injuries are common and are usually caused by traction
or pressure; individual nerves can be divided by stab wounds.
Upper Lesions of the Brachial Plexus (Erb–Duchenne Palsy) Upper
lesions of the brachial plexus are injuries resulting from excessive
displacement of the head to the opposite side and depression of the shoulder on
the same side. This causes excessive traction or even tearing of C5 and 6 roots
of the plexus. It occurs in infants during a difficult delivery or in adults
after a blow to or fall on the shoulder. The suprascapular nerve, the nerve to
the subclavius, and the musculocutaneous and axillary nerves all possess nerve
fibers derived from C5 and 6 roots and will therefore be functionless. The
following muscles will consequently be paralyzed: the supraspinatus (abductor
of the shoulder) and infraspinatus (lateral rotator of the shoulder); the subclavius
(depresses the clavicle); the biceps brachii (supinator of the forearm, flexor
of the elbow, weak flexor of the shoulder) and the greater part of the
brachialis (flexor of the elbow) and the coracobrachialis (flexes the
shoulder); and the deltoid (abductor of the shoulder) and the teres minor
(lateral rotator of the shoulder).
Thus, the limb will hang limply by the side, medially
rotated by the unopposed sternocostal part of the pectoralis major; the forearm
will be pronated because of loss of the action of the biceps. The position of
the upper limb in this condition has been likened to that of a porter or waiter
hinting for a tip. In addition, there will be a loss of sensation down the
lateral side of the arm.
Lower Lesions of the Brachial Plexus (Klumpke Palsy)
Lower lesions of the brachial plexus are usually traction
injuries caused by excessive abduction of the arm, as occurs in the case of a
person falling from a height clutching at an object to save himself or herself.
The 1st thoracic nerve is usually torn.
The nerve fibers from this segment run in the ulnar and
median nerves to supply all the small muscles of the hand. The hand has a
clawed appearance caused by hyperextension of the metacarpophalangeal joints
and flexion of the interphalangeal joints. The extensor digitorum is unopposed
by the lumbricals and interossei and extends the metacarpophalangeal joints;
the flexor digitorum superficialis and profundus are unopposed by the
lumbricals and interossei and flex the middle and terminal phalanges,
respectively.
In addition, loss of sensation will occur along the medial side
of the arm. If the 8th cervical nerve is also damaged, the extent of anesthesia
will be greater and will involve the medial side of the forearm, hand, and
medial two fingers.
Lower lesions of the brachial plexus can also be produced by
the presence of a cervical rib or malignant metastases from the lungs in the
lower deep cervical lymph nodes.
Long
Thoracic Nerve
The long thoracic nerve, which arises from C5, 6, and 7 and supplies
the serratus anterior muscle, can be injured by blows to or pressure on the
posterior triangle of the neck or during the surgical procedure of radical
mastectomy. Paralysis of the serratus anterior results in the inability to
rotate the scapula during the movement of abduction of the arm above a right
angle.
The patient therefore experiences difficulty in raising the
arm above the head. The vertebral border and inferior angle of the scapula will
no longer be kept closely applied to the chest wall and will protrude
posteriorly, a condition known as “winged scapula”

No comments:
Post a Comment