Arterial
Injury of the upper limb
The arteries of the upper limb can be damaged by penetrating
wounds or may require ligation in amputation operations.
Because of the existence of an adequate collateral
circulation around the shoulder, elbow, and wrist joints, ligation of the main arteries
of the upper limb is not followed by tissue necrosis or gangrene, provided, of
course, that the arteries forming the collateral circulation are not diseased
and the patient’s general circulation is satisfactory. Nevertheless, it can
take days or weeks for the collateral vessels to open sufficiently to provide
the distal part of the limb with the same volume of blood as previously
supplied by the main artery.
Palpation
and Compression of Arteries
A clinician must know where the arteries of the upper limb
can be palpated or compressed in an emergency. The subclavian artery, as it
crosses the first rib to become the axillary artery, can be palpated in the
root of the posterior triangle of the neck. The artery can be compressed here
against the first rib to stop a catastrophic hemorrhage. The third part of the
axillary artery can be felt in the axilla as it lies in front of the teres
major muscle. The brachial artery can be palpated in the arm as it lies on the
brachialis and is overlapped from the lateral side by the biceps brachii.
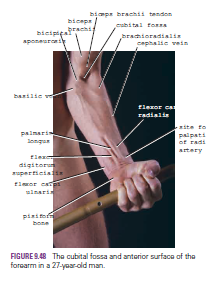
The radial artery lies superficially in front of the distal
end of the radius, between the tendons of the brachioradialis and flexor carpi
radialis; it is here that the clinician takes the radial pulse. If the pulse
cannot be felt, try feeling for the radial artery on the other wrist;
occasionally, a congenitally abnormal radial artery can be difficult to feel.
The radial artery can be less easily felt as it crosses the anatomic snuffbox.
The ulnar artery can be palpated as it crosses anterior to
the flexor retinaculum in company with the ulnar nerve. The artery lies lateral
to the pisiform bone, separated from it by the ulnar nerve. The artery is
commonly damaged here in laceration wounds in front of the wrist.
Allen
Test
The Allen test is used to determine the patency of the ulnar
and radial arteries. With the patient’s hands resting in the lap, compress the
radial arteries against the anterior surface of each radius and ask the patient
to tightly clench the fists. The clenching of the fists closes off the
superficial and deep palmar arterial arches. When the patient is asked to open
the hands, the skin of the palms is at first white, and then normally the blood
quickly flows into the arches through the ulnar arteries, causing the palms to
promptly turn pink. This establishes that the ulnar arteries are patent. The
patency of the radial arteries can be established by repeating the test but
this time compressing the ulnar arteries as they lie lateral to the pisiform
bones.
Arterial
Innervation and Raynaud’s Disease
The arteries of the upper limb are innervated by sympathetic
nerves. The preganglionic fibers originate from cell bodies in the 2nd to 8th
thoracic segments of the spinal cord. They ascend in the sympathetic trunk and
synapse in the middle cervical, inferior cervical, 1st thoracic, or stellate
ganglia. The postganglionic fibers join the nerves that form the brachial
plexus and are distributed to the arteries within the branches of the plexus.
For example, the digital arteries of the fingers are
supplied by postganglionic sympathetic fibers that run in the digital nerves. Vasospastic
diseases involving digital arterioles, such as Raynaud’s disease, may require a
cervicodorsal preganglionic sympathectomy to prevent necrosis of the fingers.
The operation is followed by arterial vasodilatation, with consequent increased
blood flow to the upper limb.