Urinary
Bladder
The urinary bladder lies immediately behind the pubic bones
inside the pelvis. Its function is storage urine and in the adult has a maximum
capacity of about 500 mL. The bladder has a strong muscular wall. Its shape and
relations vary according to the amount of urine that it contains.
When the bladder is empty it is pyramidal, having an apex, a base, and a
superior and two inferolateral surfaces; it also has a neck. in the adult lies
entirely within the pelvis; as the bladder fills, its superior wall rises up
into the hypogastric region. In the young child, the empty bladder projects
above the pelvic inlet; later, when the pelvic cavity enlarges, the bladder
sinks into the pelvis to take up the adult position.
The apex of the bladder points anteriorly and lies behind the
upper margin of the symphysis pubis. It is connected to the umbilicus by the
median umbilical ligament (remains of urachus). The base, or posterior surface
of the bladder, faces posteriorly and is triangular. The superolateral angles
are joined by the ureters, and the inferior angle gives rise to the urethra.
The two vasa deferentia lie side by side on the posterior surface of the
bladder and separate the seminal vesicles from each other. The upper part of
the posterior surface of the bladder is covered by peritoneum, which forms the
anterior wall of the rectovesical pouch. The lower part of the posterior
surface is separated from the rectum by the vasa deferentia, the seminal vesicles,
and the rectovesical fascia. The superior surface of the bladder is covered
with peritoneum and is related to coils of ileum or sigmoid colon. Along the
lateral margins of this surface, the peritoneum passes to the lateral pelvic
walls.
As the bladder fills, it becomes ovoid, and the superior surface
bulges upward into the abdominal cavity. The peritoneal covering is peeled off
the lower part of the anterior abdominal wall so that the bladder comes into
direct contact with the anterior abdominal wall.
The inferolateral surfaces are related in front to the retropubic
pad of fat and the pubic bones. More posteriorly, they lie in contact with the
obturator internus muscle above and the levator ani muscle below.
The neck of the bladder lies inferiorly and rests on the upper
surface of the prostate. Here, the smooth muscle fibers of the bladder wall are
continuous with those of the prostate. The neck of the bladder is held in position
by the puboprostatic ligaments in the male; these are called the pubovesical
ligaments in the female. These ligaments are thickenings of the pelvic fascia.
When the bladder fills, the posterior surface and neck remain more or less unchanged in position, but the superior surface rises into the abdomen The mucous membrane of the greater part of the empty bladder is thrown into folds that disappear when the bladder is full. The area of mucous membrane covering the internal surface of the base of the bladder is called the trigone. Here, the mucous membrane is always smooth, even when the viscus is empty, because the mucous membrane is firmly adherent to the underlying muscular coat. The superior angles of the trigone correspond to the openings of the ureters, and the inferior angle to the internal urethral orifice. The ureters pierce the bladder wall obliquely, and this provides a valvelike action, which prevents a reverse flow of urine toward the kidneys
When the bladder fills, the posterior surface and neck remain more or less unchanged in position, but the superior surface rises into the abdomen The mucous membrane of the greater part of the empty bladder is thrown into folds that disappear when the bladder is full. The area of mucous membrane covering the internal surface of the base of the bladder is called the trigone. Here, the mucous membrane is always smooth, even when the viscus is empty, because the mucous membrane is firmly adherent to the underlying muscular coat. The superior angles of the trigone correspond to the openings of the ureters, and the inferior angle to the internal urethral orifice. The ureters pierce the bladder wall obliquely, and this provides a valvelike action, which prevents a reverse flow of urine toward the kidneys
as the bladder fills. The trigone is limited above by a
muscular ridge, which runs from the opening of one ureter to that of the other and
is known as the interureteric ridge. The uvula vesicae is a small elevation
situated immediately behind the urethral orifice, which is produced by the
underlying median lobe of the prostate.
The muscular coat of the bladder is composed of smooth
muscle and is arranged as three layers of interlacing bundles known as the
detrusor muscle. At the neck of the bladder, the circular component of the
muscle coat is thickened to form the sphincter vesicae.
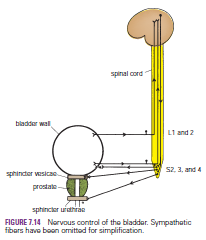
Micturition
Micturition is a reflex action that, in the toilet-trained
individual, is controlled by higher centers in the brain. The reflex is
initiated when the volume of urine reaches about 300 mL; stretch receptors in
the bladder wall are stimulated and transmit impulses to the central nervous
system, and the individual has a conscious desire to micturate. Most afferent impulses
pass up the pelvic splanchnic nerves and enter the 2nd, 3rd, and 4th sacral
segments of the spinal cord. Some afferent impulses travel with the sympathetic
nerves via the hypogastric plexuses and enter the first and second lumbar
segments of the spinal cord. Efferent parasympathetic impulses leave the cord
from the second, third, and fourth sacral segments and pass via the
parasympathetic preganglionic nerve fibers through the pelvic splanchnic nerves
and the inferior hypogastric plexuses to the bladder wall, where they synapse
with postganglionic neurons. By means of this nervous pathway, the smooth
muscle of the bladder wall (the detrusor muscle) is made to contract, and the
sphincter vesicae is made to relax. Efferent impulses also pass to the urethral
sphincter via the pudendal nerve (S2, 3, and 4), and this undergoes relaxation.
Once urine enters the urethra, additional afferent impulses pass to the spinal
cord from the urethra and reinforce the reflex action. Micturition can be
assisted by contraction of the abdominal muscles to raise the intra-abdominal
and pelvic pressures and exert external pressure on the bladder. In young
children, micturition is a simple reflex act and takes place whenever the
bladder becomes distended. In the adult, this simple stretch reflex is
inhibited by the activity of the cerebral cortex until the time and place for
micturition are favorable. The inhibitory fibers pass downward with the
corticospinal tracts to the 2nd, 3rd, and 4th sacral segments of the cord.
Voluntary control of micturition is accomplished by contracting the sphincter
urethrae, which closes the urethra; this is assisted by the sphincter vesicae, which
compresses the bladder neck. Voluntary control of micturition is normally
developed during the second or third year of life.



No comments:
Post a Comment